Question 1:
Which of the following is the mechanism of action of polyenes?
A) Inhibition of (1,3)-β-D-glucan synthase
B) Inhibition of lanosterol 14α-demethylase
C) Inhibition of squalene epoxidase
D) Binding to ergosterol in fungal cell membranes, forming pores
E) Inhibition of microtubule function
Click here to see the answer
Correct Answer: D) Binding to ergosterol in fungal cell membranes, forming pores
Explanation: Polyenes, such as amphotericin B and nystatin, bind to ergosterol in fungal cell membranes, leading to pore formation and cell lysis.
Question 2:
Which antifungal is primarily used for superficial infections such as oral thrush and is administered as a swish, swirl, and swallow?
A) Fluconazole
B) Nystatin
C) Amphotericin B
D) Caspofungin
E) Terbinafine
Click here to see the answer
Correct Answer: B) Nystatin
Explanation: Nystatin is a topical/oral antifungal used for superficial infections like oral thrush. It has poor gastrointestinal absorption and is used in a swish, swirl, and swallow method for oral candidiasis.
Question 3:
Which of the following antifungal classes inhibits the enzyme lanosterol 14α-demethylase, blocking ergosterol synthesis?
A) Azoles
B) Polyenes
C) Echinocandins
D) Pyrimidine Analogs
E) Allylamines
Click here to see the answer
Correct Answer: A) Azoles
Explanation: Azoles inhibit lanosterol 14α-demethylase, an enzyme involved in ergosterol synthesis, disrupting the fungal cell membrane.
Question 4:
Which of the following antifungals is a triazole used for systemic fungal infections?
A) Clotrimazole
B) Miconazole
C) Fluconazole
D) Terbinafine
E) Griseofulvin
Click here to see the answer
Correct Answer: C) Fluconazole
Explanation: Fluconazole is a triazole antifungal primarily used for systemic infections, unlike imidazoles such as clotrimazole and miconazole, which are used for superficial infections.
Question 5:
Which echinocandin is commonly used for invasive candidiasis and aspergillosis?
A) Terbinafine
B) Caspofungin
C) Fluconazole
D) Griseofulvin
E) Nystatin
Click here to see the answer
Correct Answer: B) Caspofungin
Explanation: Caspofungin is an echinocandin used for invasive candidiasis and aspergillosis by inhibiting the enzyme (1,3)-β-D-glucan synthase, crucial for fungal cell wall synthesis.
Question 6:
Which of the following antifungals inhibits squalene epoxidase, affecting ergosterol synthesis?
A) Amphotericin B
B) Micafungin
C) Voriconazole
D) Terbinafine
E) Flucytosine
Click here to see the answer
Correct Answer: D) Terbinafine
Explanation: Terbinafine is an allylamine that inhibits squalene epoxidase, an enzyme critical for ergosterol synthesis in fungal cells, making it effective for dermatophyte infections.
Question 7:
Which antifungal is used in combination with amphotericin B for systemic infections such as cryptococcal meningitis?
A) Caspofungin
B) Griseofulvin
C) Flucytosine
D) Tolnaftate
E) Miconazole
Click here to see the answer
Correct Answer: C) Flucytosine
Explanation: Flucytosine is a pyrimidine analog used in combination with amphotericin B for systemic fungal infections like cryptococcal meningitis.
Question 8:
Which antifungal disrupts microtubule function, inhibiting fungal cell division, and is used for dermatophyte infections?
A) Griseofulvin
B) Nystatin
C) Caspofungin
D) Fluconazole
E) Amphotericin B
Click here to see the answer
Correct Answer: A) Griseofulvin
Explanation: Griseofulvin disrupts microtubule function, inhibiting fungal cell division, and is used for dermatophyte infections such as tinea capitis.
Question 9:
Which antifungal is commonly used for topical treatment of tinea infections, such as athlete’s foot?
A) Caspofungin
B) Tolnaftate
C) Voriconazole
D) Terbinafine
E) Flucytosine
Click here to see the answer
Correct Answer: B) Tolnaftate
Explanation: Tolnaftate is a topical antifungal used for treating tinea infections, such as athlete’s foot.
Question 10:
Which antifungal has poor gastrointestinal absorption and is primarily used for superficial infections like oral thrush and vaginal candidiasis?
A) Amphotericin B
B) Nystatin
C) Caspofungin
D) Fluconazole
E) Terbinafine
Click here to see the answer
Correct Answer: B) Nystatin
Explanation: Nystatin is poorly absorbed through the gastrointestinal tract and is used for superficial fungal infections like oral thrush and vaginal candidiasis.
Question 11: Amphotericin B for Invasive Fungal Infections
A 60-year-old man is admitted to the hospital with a diagnosis of invasive aspergillosis. Due to the severity of the infection, the physician prescribes liposomal amphotericin B (Ambisome) at a dose of 5 mg/kg/day. The patient asks the pharmacist about the side effects of this medication, especially since he has heard that amphotericin B can be toxic.
Question 1:
What should the pharmacist inform the patient regarding the difference in toxicity between conventional amphotericin B and liposomal amphotericin B?
A) Liposomal amphotericin B has the same toxicity profile as conventional amphotericin B.
B) Liposomal amphotericin B is associated with a significantly lower risk of nephrotoxicity compared to conventional amphotericin B.
C) Liposomal amphotericin B is more nephrotoxic than conventional amphotericin B.
D) Liposomal amphotericin B is only effective for mild fungal infections and has fewer side effects overall.
E) Both forms of amphotericin B cause severe hepatotoxicity rather than nephrotoxicity.
Click here to see the answer
Correct Answer:
B) Liposomal amphotericin B is associated with a significantly lower risk of nephrotoxicity compared to conventional amphotericin B.
Explanation:
Liposomal amphotericin B (Ambisome) is formulated to reduce nephrotoxicity and infusion-related reactions compared to conventional amphotericin B deoxycholate. The lipid-based formulation encapsulates the drug, delivering it more selectively to infected tissues, thereby reducing kidney toxicity.
Follow-Up Question:
What is a common infusion-related reaction that patients may experience during amphotericin B therapy?
A) Hypoglycemia
B) Fever, chills, and rigors
C) Bradycardia
D) Constipation
E) Euphoria
Click here to see the answer
Correct Answer:
B) Fever, chills, and rigors
Explanation:
Infusion-related reactions, including fever, chills, and rigors, are common with amphotericin B therapy. These reactions are most pronounced with conventional formulations and may require premedication with antipyretics or corticosteroids to manage.
Question 12: Nystatin for Oral Candidiasis
A 45-year-old woman with poorly controlled diabetes presents to her physician with white patches on her tongue and inner cheeks, which are diagnosed as oral candidiasis (thrush). She is prescribed nystatin oral suspension at a dose of 500,000 units four times daily. The patient asks the pharmacist how to use the medication effectively.
Question 1:
How should the pharmacist counsel the patient on the correct use of nystatin oral suspension for oral candidiasis?
A) Swish and swallow the suspension, making sure to hold it in the mouth for several minutes before swallowing.
B) Swallow the suspension immediately without holding it in the mouth.
C) Apply the suspension to the skin around the mouth instead of swallowing it.
D) Gargle with the suspension and then spit it out.
E) Dilute the suspension with water before use.
Click here to see the answer
Correct Answer:
A) Swish and swallow the suspension, making sure to hold it in the mouth for several minutes before swallowing.
Explanation:
The nystatin suspension should be swished around the mouth for several minutes to ensure adequate contact with the affected areas before swallowing. This helps to treat the oral candidiasis more effectively by maintaining exposure to the antifungal agent.
Follow-Up Question:
What is a common side effect that the patient should be aware of when using nystatin oral suspension?
A) Severe diarrhea
B) Gastrointestinal upset
C) Hypokalemia
D) Nephrotoxicity
E) Hypertension
Click here to see the answer
Correct Answer:
B) Gastrointestinal upset
Explanation:
Nystatin oral suspension is generally well-tolerated, but mild gastrointestinal upset, such as nausea or diarrhea, may occur. It is not systemically absorbed, so systemic side effects are uncommon. This means that if someone accidentally swallows nystatin in a considerable amount, it is not a reason to panic. Just wait and watch for the symptoms of gastric upset.
Question 13
What is the typical oral dosing for Ketoconazole in systemic fungal infections?
A) 100-200 mg daily
B) 150-250 mg daily
C) 200-400 mg daily
D) 300-500 mg daily
E) 400-600 mg daily
Click here to see the answer
Correct Answer: C) 200-400 mg daily
Explanation: Ketoconazole is rarely used systemically due to side effects, but the oral dosing is 200-400 mg daily for systemic fungal infections.
Question 14
Which of the following is a serious side effect of systemic Ketoconazole use?
A) Nephrotoxicity
B) Hepatotoxicity
C) Hyperglycemia
D) Cardiotoxicity
E) Hypokalemia
Click here to see the answer
Correct Answer: B) Hepatotoxicity
Explanation: Systemic use of Ketoconazole can cause hepatotoxicity, adrenal insufficiency, and QT prolongation.
Question 15
For what conditions is Ketoconazole primarily used topically?
A) Onychomycosis and athlete’s foot
B) Psoriasis and eczema
C) Seborrheic dermatitis, dandruff, and cutaneous fungal infections
D) Bacterial vaginosis and acne
E) Viral infections and keratitis
Click here to see the answer
Correct Answer: C) Seborrheic dermatitis, dandruff, and cutaneous fungal infections
Explanation: Ketoconazole is primarily used topically for conditions like seborrheic dermatitis, dandruff, and fungal skin infections.
Question 16
Which of the following is a common use of Clotrimazole lozenges?
A) Treatment of onychomycosis
B) Treatment of oral thrush
C) Treatment of bacterial vaginosis
D) Treatment of athlete’s foot
E) Treatment of seborrheic dermatitis
Click here to see the answer
Correct Answer: B) Treatment of oral thrush
Explanation: Clotrimazole lozenges are commonly used for treating oral thrush (candidiasis).
Question 17
What is the correct dosing regimen for Clotrimazole lozenges in the treatment of oral thrush?
A) 5 mg lozenge twice daily
B) 10 mg lozenge 3 times daily
C) 10 mg lozenge 5 times daily
D) 20 mg lozenge once daily
E) 50 mg lozenge 4 times daily
Click here to see the answer
Correct Answer: C) 10 mg lozenge 5 times daily
Explanation: Clotrimazole lozenges are dosed at 10 mg dissolved in the mouth 5 times daily for the treatment of oral thrush.
Question 18
Which antifungal is typically used for treating vaginal yeast infections, oral thrush, and cutaneous fungal infections?
A) Fluconazole
B) Clotrimazole
C) Itraconazole
D) Econazole
E) Miconazole
Click here to see the answer
Correct Answer: B) Clotrimazole
Explanation: Clotrimazole is used for the treatment of vaginal yeast infections, oral thrush, and various cutaneous fungal infections.
Question 19
What is a common side effect associated with topical use of Miconazole?
A) Dry skin
B) Hair loss
C) Local irritation, burning, or redness
D) Hypotension
E) Weight gain
Click here to see the answer
Correct Answer: C) Local irritation, burning, or redness
Explanation: Miconazole commonly causes local irritation, burning, or redness when applied topically.
Question 20
Which enzyme do Ketoconazole, Clotrimazole, and Miconazole inhibit, potentially causing drug interactions?
A) CYP1A2
B) CYP2D6
C) CYP2C19
D) CYP3A4
E) CYP2C9
Click here to see the answer
Correct Answer: D) CYP3A4
Explanation: Ketoconazole, Clotrimazole, and Miconazole are all inhibitors of CYP3A4, which can lead to significant drug interactions.
Question 21
What is the main use of Econazole in antifungal therapy?
A) Treating systemic fungal infections
B) Treating tinea pedis, tinea corporis, and tinea cruris
C) Treating bacterial infections
D) Treating onychomycosis
E) Treating viral infections
Click here to see the answer
Correct Answer: B) Treating tinea pedis, tinea corporis, and tinea cruris
Explanation: Econazole is commonly used topically for the treatment of fungal infections such as athlete’s foot, ringworm, and jock itch.
Question 22
What is a key characteristic of Ketoconazole that limits its systemic use?
A) High bioavailability
B) Risk of hepatotoxicity and adrenal insufficiency
C) Low risk of drug interactions
D) Ability to treat viral infections
E) Excellent absorption
Click here to see the answer
Correct Answer: B) Risk of hepatotoxicity and adrenal insufficiency
Explanation: Ketoconazole is rarely used systemically due to the risk of serious side effects such as hepatotoxicity and adrenal insufficiency.
Question 23:
Which formulation of fluconazole is available for administration?
A) Oral tablets
B) Oral suspension
C) IV
D) Oral powder
E) All of the above
Click here to see the answer
Correct Answer: E) All of the above
Explanation: Fluconazole is available in oral tablets, oral suspension, and intravenous (IV) formulations, making it versatile for different routes of administration.
Question 24:
Fluconazole is preferred for which type of fungal infections?
A) Candida infections (except Candida krusei and Candida glabrata)
B) Invasive aspergillosis
C) Mucormycosis
D) Histoplasmosis
E) Tinea capitis
Click here to see the answer
Correct Answer: A) Candida infections (except Candida krusei and Candida glabrata)
Explanation: Fluconazole is commonly used for Candida infections but is ineffective against Candida krusei and Candida glabrata. It is also used for cryptococcal meningitis and prophylaxis in immunocompromised patients.
Question 25:
Which of the following is a black box warning for itraconazole?
A) Hepatotoxicity
B) Heart failure
C) Visual disturbances
D) Hallucinations
E) Photosensitivity
Click here to see the answer
Correct Answer: B) Heart failure
Explanation: Itraconazole carries a black box warning for use in patients with ventricular dysfunction, including heart failure, due to the risk of exacerbating this condition.
Question 26:
Which antifungal is first-line treatment for invasive aspergillosis?
A) Fluconazole
B) Voriconazole
C) Itraconazole
D) Posaconazole
E) Isavuconazole
Click here to see the answer
Correct Answer: B) Voriconazole
Explanation: Voriconazole is the first-line treatment for invasive aspergillosis and other serious fungal infections.
Question 27:
What is a notable side effect of voriconazole?
A) Visual disturbances (blurred vision, photophobia)
B) Heart failure
C) Rhabdomyolysis
D) Hypotension
E) Hematuria
Click here to see the answer
Correct Answer: A) Visual disturbances (blurred vision, photophobia)
Explanation: Voriconazole is associated with visual disturbances such as blurred vision and photophobia, as well as other side effects including hepatotoxicity and QT prolongation.
Question 28:
Which triazole antifungal is mainly used for prophylaxis of invasive fungal infections in high-risk patients?
A) Fluconazole
B) Posaconazole
C) Voriconazole
D) Isavuconazole
E) Itraconazole
Click here to see the answer
Correct Answer: B) Posaconazole
Explanation: Posaconazole is primarily used for the prophylaxis of invasive fungal infections in high-risk patients, such as those undergoing chemotherapy or bone marrow transplantation.
Question 29:
Which antifungal has fewer drug-drug interactions and a lower risk of QT prolongation compared to other triazoles?
A) Fluconazole
B) Voriconazole
C) Itraconazole
D) Posaconazole
E) Isavuconazole
Click here to see the answer
Correct Answer: E) Isavuconazole
Explanation: Isavuconazole is known for having fewer drug-drug interactions and a lower risk of QT prolongation compared to other triazoles, making it a safer option for some patients.
Question 30:
Which enzyme(s) do fluconazole and voriconazole inhibit, leading to potential drug-drug interactions?
A) CYP2C9 and CYP2C19
B) CYP3A4
C) CYP1A2
D) Both A and B
E) None of the above
Click here to see the answer
Correct Answer: D) Both A and B
Explanation: Fluconazole and voriconazole inhibit CYP2C9, CYP2C19, and CYP3A4, which can lead to increased levels of co-administered drugs metabolized by these enzymes, such as warfarin and statins.
Question 31:
Which of the following triazoles is preferred for the treatment of cryptococcal meningitis?
A) Fluconazole
B) Voriconazole
C) Itraconazole
D) Posaconazole
E) Isavuconazole
Click here to see the answer
Correct Answer: A) Fluconazole
Explanation: Fluconazole is commonly used as a first-line treatment for cryptococcal meningitis, especially in immunocompromised patients.
Question 32:
Which of the following triazoles requires an acidic environment for absorption when administered in capsule form?
A) Fluconazole
B) Voriconazole
C) Itraconazole
D) Posaconazole
E) Isavuconazole
Click here to see the answer
Correct Answer: C) Itraconazole
Explanation: Itraconazole capsules require an acidic environment for proper absorption. The oral solution form is preferred for better absorption, especially in patients taking acid-suppressing medications.
Question 33:
Ketoconazole shampoo is used primarily for the treatment of which conditions?
A) Acne
B) Psoriasis
C) Dandruff and Seborrheic Dermatitis
D) Eczema
E) Rosacea
Click here to see the answer
Correct Answer: C) Dandruff and Seborrheic Dermatitis
Explanation: Ketoconazole shampoo is commonly used to treat dandruff and seborrheic dermatitis due to its antifungal properties.
Question 34:
Ketoconazole is a potent substrate and inhibitor of which enzyme?
A) CYP2C9
B) CYP3A4
C) CYP1A2
D) CYP2D6
E) P-gp
Click here to see the answer
Correct Answer: B) CYP3A4
Explanation: Ketoconazole is a potent substrate and inhibitor of CYP3A4, which can lead to significant drug-drug interactions with other medications metabolized by this enzyme.
Question 35:
Clotrimazole is the drug of choice for which conditions?
A) Athlete’s Foot, Vaginal Candidiasis, and Complicated Diaper Rash
B) Seborrheic Dermatitis and Dandruff
C) Onychomycosis and Tinea Versicolor
D) Psoriasis and Eczema
E) Acne and Rosacea
Click here to see the answer
Correct Answer: A) Athlete’s Foot, Vaginal Candidiasis, and Complicated Diaper Rash
Explanation: Clotrimazole is the drug of choice for treating athlete’s foot (tinea pedis), vaginal candidiasis, and complicated diaper rash due to its broad antifungal activity.
Question 36:
What is the first-line treatment for dandruff and seborrhea?
A) Itraconazole 1% cream
B) Clotrimazole 2% cream
C) Ketoconazole 2% cream or shampoo
D) Terbinafine 1% gel
E) Miconazole 2% cream
Click here to see the answer
Correct Answer: C) Ketoconazole 2% cream or shampoo
Explanation: Ketoconazole 2% cream and shampoo are considered first-line treatments for dandruff and seborrheic dermatitis due to their antifungal and anti-inflammatory properties.
Question 37:
Itraconazole is commonly used as an oral treatment for which condition?
A) Seborrheic Dermatitis
B) Vaginal Candidiasis
C) Onychomycosis
D) Athlete’s Foot
E) Tinea Capitis
Click here to see the answer
Correct Answer: C) Onychomycosis
Explanation: Itraconazole is commonly used as an oral antifungal treatment for onychomycosis (fungal nail infections), particularly when topical treatments are ineffective.
Question 38:
Which of the following is an alternative topical treatment for onychomycosis?
A) Ketoconazole 2% cream
B) Clotrimazole 1% cream
C) Efinaconazole 10% topical solution (Jublia)
D) Fluconazole oral suspension
E) Terbinafine 1% gel
Click here to see the answer
Correct Answer: C) Efinaconazole 10% topical solution (Jublia)
Explanation: Efinaconazole 10% topical solution (Jublia) is an alternative topical treatment for onychomycosis, particularly in patients who cannot tolerate or prefer not to use oral antifungals.
Question 39:
Itraconazole is metabolized into which active metabolite?
A) Hydroxy-fluconazole
B) Hydroxy-terbinafine
C) Hydroxy-itraconazole
D) Hydroxy-ketoconazole
E) Hydroxy-voriconazole
Click here to see the answer
Correct Answer: C) Hydroxy-itraconazole
Explanation: Itraconazole is metabolized into hydroxy-itraconazole, which is also a potent inhibitor of CYP3A4 and P-glycoprotein (P-gp).
Question 40:
Itraconazole oral capsules are primarily used for which condition?
A) Tinea Versicolor
B) Onychomycosis
C) Seborrheic Dermatitis
D) Athlete’s Foot
E) Vaginal Candidiasis
Click here to see the answer
Correct Answer: B) Onychomycosis
Explanation: Itraconazole oral capsules are commonly prescribed for the treatment of onychomycosis (fungal nail infections).
Question 41:
Which of the following is both a substrate and inhibitor of CYP3A4?
A) Clotrimazole
B) Fluconazole
C) Itraconazole
D) Ketoconazole
E) Voriconazole
Click here to see the answer
Correct Answer: C) Itraconazole
Explanation: Itraconazole is both a substrate and a potent inhibitor of CYP3A4, leading to potential drug-drug interactions with other medications metabolized by this enzyme.
Question 42
What is the standard oral dosing regimen of Terbinafine for toenail onychomycosis?
A) 100 mg daily for 4 weeks
B) 150 mg daily for 8 weeks
C) 200 mg daily for 6 weeks
D) 250 mg daily for 12 weeks
E) 300 mg daily for 10 weeks
Click here to see the answer
Correct Answer: D) 250 mg daily for 12 weeks
Explanation: The standard oral dosing for toenail onychomycosis is 250 mg of Terbinafine once daily for 12 weeks.
Question 43
Which of the following is a common side effect of oral Terbinafine?
A) Hepatotoxicity
B) Stevens-Johnson syndrome
C) Gastrointestinal upset
D) Neutropenia
E) Severe allergic reactions
Click here to see the answer
Correct Answer: C) Gastrointestinal upset
Explanation: While hepatotoxicity and severe allergic reactions are possible, gastrointestinal upset (nausea, diarrhea) is a more common side effect of oral Terbinafine.
Question 44
Which of the following drugs could be affected by the CYP2D6 inhibitory effects of Terbinafine?
A) Ibuprofen
B) Fluoxetine
C) Omeprazole
D) Lisinopril
E) Metformin
Click here to see the answer
Correct Answer: B) Fluoxetine
Explanation: Terbinafine is a moderate inhibitor of CYP2D6, which can increase the levels of drugs metabolized by this enzyme, such as fluoxetine (an SSRI).
Question 45
In which of the following conditions is oral Terbinafine contraindicated?
A) Hepatic impairment
B) Heart failure
C) Hypertension
D) Asthma
E) Depression
Click here to see the answer
Correct Answer: A) Hepatic impairment
Explanation: Oral Terbinafine is contraindicated in patients with hepatic impairment due to the risk of hepatotoxicity.
Question 46
Which of the following should be monitored in patients on long-term oral Terbinafine therapy?
A) Renal function
B) Blood pressure
C) Serum calcium levels
D) Liver function
E) Cholesterol levels
Click here to see the answer
Correct Answer: D) Liver function
Explanation: Due to the risk of hepatotoxicity, liver function should be monitored before and during long-term oral Terbinafine therapy.
Question 47
What is the typical dosing regimen for Flucytosine in the treatment of severe fungal infections?
A) 100-200 mg/day divided into 2 doses
B) 250-500 mg/day divided into 3 doses
C) 50-150 mg/kg/day divided into 4 doses
D) 500-1000 mg/day divided into 2 doses
E) 2000 mg/day in a single dose
Click here to see the answer
Correct Answer: C) 50-150 mg/kg/day divided into 4 doses
Explanation: Flucytosine is dosed at 50-150 mg/kg/day divided into 4 doses, depending on the severity of infection and renal function. It is typically used in combination therapy to reduce resistance development.
Question 48
Which of the following is a common side effect of Flucytosine?
A) Hyperkalemia
B) Bone marrow suppression
C) Hypertension
D) Peripheral neuropathy
E) Hyperglycemia
Click here to see the answer
Correct Answer: B) Bone marrow suppression
Explanation: Bone marrow suppression, which may result in leukopenia, thrombocytopenia, and anemia, is a common hematologic side effect of Flucytosine.
Question 49
Flucytosine is commonly used in combination with which of the following drugs for treating cryptococcal meningitis?
A) Voriconazole
B) Itraconazole
C) Amphotericin B
D) Caspofungin
E) Terbinafine
Click here to see the answer
Correct Answer: C) Amphotericin B
Explanation: Flucytosine is commonly used in combination with Amphotericin B for the treatment of cryptococcal meningitis, as this combination improves efficacy and reduces resistance development.
Question 50
Which of the following monitoring parameters is most important during Flucytosine therapy?
A) Blood pressure
B) Blood glucose levels
C) Complete Blood Count (CBC)
D) Serum potassium
E) Electrocardiogram (ECG)
Click here to see the answer
Correct Answer: C) Complete Blood Count (CBC)
Explanation: Regular monitoring of CBC is essential during Flucytosine therapy to detect early signs of bone marrow suppression.
Question 51
Flucytosine requires dose adjustment in which patient population?
A) Patients with hepatic impairment
B) Patients with bone marrow suppression
C) Patients with renal impairment
D) Patients with hyperlipidemia
E) Patients with hypertension
Click here to see the answer
Correct Answer: C) Patients with renal impairment
Explanation: Flucytosine requires dose adjustment in patients with renal impairment to avoid drug accumulation and potential toxicity, particularly nephrotoxicity.
Question 52
A 65-year-old woman is prescribed itraconazole to treat a fungal toenail infection. She has a history of hypertension, controlled with an ACE inhibitor, and high cholesterol, for which she takes atorvastatin 40 mg daily. The patient is concerned about possible drug interactions with her new medication.
Question 1:
What potential risk exists when combining itraconazole with atorvastatin?
A) Increased blood pressure
B) Risk of gastrointestinal discomfort
C) Higher risk of muscle toxicity, including myopathy or rhabdomyolysis
D) Reduced effectiveness of atorvastatin
E) Increased blood sugar levels
Click here to see the answer
Correct Answer:
C) Higher risk of muscle toxicity, including myopathy or rhabdomyolysis
Explanation:
Itraconazole is a potent inhibitor of the CYP3A4 enzyme, which is responsible for metabolizing atorvastatin. When these two medications are combined, it can result in elevated atorvastatin levels in the bloodstream, which increases the risk of serious side effects such as myopathy and rhabdomyolysis.
Follow-Up Question:
What action should the healthcare provider take to manage the risk of this interaction?
A) Continue both medications and monitor for muscle symptoms.
B) Stop the ACE inhibitor to avoid complications.
C) Consider reducing the atorvastatin dose or switching to a statin not metabolized by CYP3A4, such as pravastatin or rosuvastatin.
D) Advise the patient to take the medications at different times of the day.
E) Increase the atorvastatin dose to maintain cholesterol control.
Click here to see the answer
Correct Answer:
C) Consider reducing the atorvastatin dose or switching to a statin not metabolized by CYP3A4, such as pravastatin or rosuvastatin.
Explanation:
To mitigate the risk of muscle toxicity, the provider should either lower the dose of atorvastatin or switch to a statin that is not metabolized by CYP3A4. Rosuvastatin and pravastatin are appropriate alternatives that are less likely to interact with itraconazole.
Question 53
A 40-year-old man visits the pharmacy with a prescription for ketoconazole 2% shampoo to treat his seborrheic dermatitis. He asks the pharmacist how to use the shampoo properly and if there are any side effects or precautions he should be aware of.
Question 1:
What instructions should the pharmacist provide to the patient regarding the proper use of ketoconazole shampoo?
A) Apply the shampoo to dry hair and scalp, leave it on for 30 seconds, and rinse immediately.
B) Apply the shampoo to wet hair and scalp, leave it on for 5 minutes, and then rinse thoroughly.
C) Use the shampoo once a month to prevent symptoms from worsening.
D) Apply the shampoo only to the affected areas and rinse after 1 minute.
E) Use the shampoo every day for the first week and then reduce to twice daily.
Click here to see the answer
Correct Answer:
B) Apply the shampoo to wet hair and scalp, leave it on for 5 minutes, and then rinse thoroughly.
Explanation:
Ketoconazole shampoo should be applied to wet hair and scalp, massaged into the scalp, and left on for about 5 minutes before rinsing thoroughly. This allows enough contact time for the medication to work effectively against the fungal infection.
Follow-Up Question:
What should the pharmacist advise the patient regarding the potential side effects of ketoconazole shampoo?
A) The shampoo can cause dizziness and fatigue.
B) The shampoo may cause local irritation, burning, or itching of the scalp.
C) The shampoo can lead to systemic side effects, including hepatotoxicity.
D) The shampoo will cause hair loss if used frequently.
E) The shampoo can cause gastrointestinal upset.
Click here to see the answer
Correct Answer:
B) The shampoo may cause local irritation, burning, or itching of the scalp.
Explanation:
Common side effects of ketoconazole shampoo include local irritation, burning, or itching of the scalp. These side effects are usually mild and self-limiting. Systemic side effects are very rare since the shampoo is used topically.
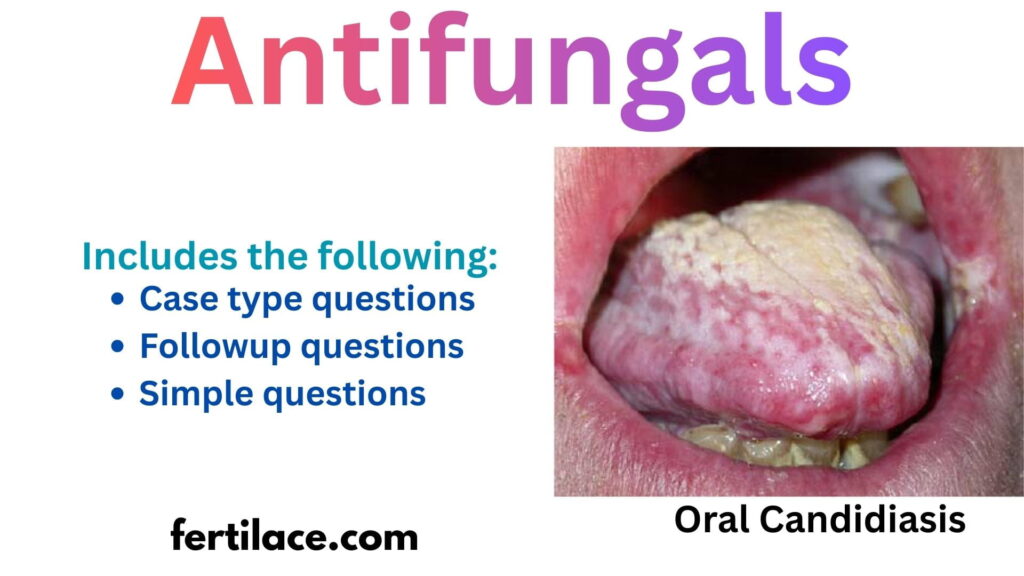
Image source
The photo of oral candidiasis in the cover image is taken from here, and it’s shared under Creative Commons CC0 1.0 Universal Public Domain Dedication. The details mentioned below are associated with the photo.
| Description | English: Oral pseudomembranous candidiasis on the dorsum of the tongue |
| Date | 10 June 2005 |
| Source | https://www.researchgate.net/publication/7794502_Effect_of_fluconazole_antifungal_prophylaxis_on_oral_mucositis_in_head_and_neck_cancer_patients_receiving_radiotherapy |
| Author | Ourania Nicolatou-Galitis et al. |