Semen analysis
Semen analysis is performed for the evaluation of fertility disorders. The symptoms of androgen deficiency may or may not be observed.
The purpose of writing this article is to help understand the semen analysis report for individuals who are not familiar with medical terminologies. All the technical terms have been simplified and explained.
Table of Contents
Semen analysis is done to evaluate the following parameters:
- Semen volume
- pH
- Total sperm count
- Sperm motility
- Sperm morphology
- WBC (White Blood Cells)
- Fructose
Things to consider for semen collection
- Patients should observe a period of abstinence of between 48 hours and 7 days.
- The ejaculate should be obtained at the clinic or lab in a suitable room.
- This eliminates the effect of temperature and time taken to transport the sample to clinic or lab.
- The room should contain appropriate illustrated literature, background music, or video recordings.
- The sample should be produced by masturbation into a clean, wide-mouthed graduated glass- container.
- All of the ejaculate should be collected in the container since total semen volume is one of the evaluating parameters.
- The estimation of fertility potential should be done after 2 or 3 semen analyses.
What does a sperm analysis tell?
Sperm analysis or semen analysis is used to estimate the fertility potential of a male.
Some additional tests like ultrasound scans, testicular biopsies, and hormonal evaluation might be advised in some cases.
How to read and interpret semen analysis report
Macroscopic evaluation parameters
Colour
- Grey-opalescent appearance – indicative of a normal ejaculate.
- Whitish color – may indicate high sperm numbers or the presence of leukocytes.
- Yellowish colour with a purulent smell indicates the possibility of infections.
- Reddish-brown colour – indicates the presence of red blood cells.
Semen volume
Semen volume of more than 1.5 ml is considered normal.
A Semen volume of less than 1.5 ml (normal value) may be indicative of the following:
- Retrograde ejaculation
- Abnormities of the vas deferens or seminal vesicles
- Ejaculatory duct obstruction
- Hypogonadism, and
- Sympathetic dysfunction
Low semen volume is possible because of incomplete collection.
Sperm agglutination and sperm aggregation
Sperm aggregation
Most likely you will not see this term in any semen analysis report. When immotile sperm cells stick to each other or other elements of ejaculate, then it is called sperm aggregation. Since these sperm cells are immotile and cannot contribute towards fertility, they do not hold much clinical significance.
Sperm agglutination
This refers to the sticking or union of motile sperm cells with each other. This is indicative of anti-sperm antibodies. A mixed Agglutination Reaction (MAR) test should be recommended to detect anti-sperm antibodies.
| Grade | Parameter | Analysis |
| Grade 1 (isolated) | Less than 10 spermatozoa per agglutinate, many mobile sperm | Indicative of fertility |
| Grade 2 (moderate) | 10–50 spermatozoa per agglutinate, many mobile sperm | Indicative of fertility |
| Grade 3 (strong) | agglutinates with >50 spermatozoa, only few mobile spermatozoa | Indicates a possible infertility |
| Grade 4 (complete) | completely agglutinated spermatozoa, no mobile spermatozoa visible | Indicates infertility |
pH
- pH of the semen should be slightly alkaline, which is more than 7.2 but less than 8.
- An acidic seminal pH in patients with azoospermia may indicate obstruction of the epididymis, the deferent ducts, the seminal vesicles, or the ejaculatory ducts.
- An alkaline pH (>8) measured soon after liquefaction may indicate the presence of infection.
Viscosity and Liquefaction time
Semen is initially a coagulum that liquefies after some time. Normal liquefaction time for semen is between 5 to 25 minutes. In liquefied state, semen can be poured drop by drop. If a coagulum is not initially present, then obstruction of the ejaculatory ducts or absence of the seminal vesicles can be suspected. Failure of liquefaction, on the other hand, may indicate inadequate secretion of prostatic proteolytic enzymes.
Microscopic evaluation of semen
Total sperm count
The total sperm count in an ejaculate should be more than or equal to 39 million. If it is less than that, then it’s indicative of male-factor infertility.
Sperm Concentration
Sperm concentration refers to sperm density. The normal range is 15 million per ml of semen.
- Oligozoospermia or Oligospermia – When there are less than 15 million sperm cells per ml, the condition is called oligozoospermia.
- Azoospermia – When there are zero sperm cells in an ejaculate, the condition is called azoospermia.
Note:
Consider this scenario: A patient has a semen volume of 2 ml and sperm concentration is 16 million per ml. This gives the total sperm count at 32 million which is less than the normal value of 39 million. Hence, this can be considered a case of borderline infertility.
Sperm motility
The normal value for sperm motility is 40% (minimum).
The normal value for forward progressive sperm motility is 32% (minimum).
Types of motility:
- Progressive motility – This is the term used when sperms travel some distance in a linear direction or in circular arcs. Note that only progressively motile sperms contribute towards fertility.
- Non-progressive motility – This is the term used when sperms move in one place but do not travel any distance. This is more like moving on one spot or moving in a small circular path.
- Immotile – This is the term used when there is no movement of sperm cells.
Another term that you may find in a semen analysis report is ‘pinhead sperms‘. These are only sperm tails (sperm cells without the head) and can be very motile. These cells do not contribute towards fertility since they don’t have a head that carries genetic information.
Asthenozoospermia or asthenospermia is the term used when sperm motility is less than the normal values of motility. Absolute asthenozoospermia is the term used when the sample has zero motile sperms.
- If the semen sample was analyzed using CASA (computer-assisted semen analysis) you might see these terms in the report. I am mentioning these terms for your reference only. These are VCL (curvilinear velocity (µm/s)), VAP (averaged path velocity (µm/s)), VSL (straight-line velocity (µm/s)), ALH (amplitude of lateral head displacement (µm)), MAD (mean angular displacement (°)). Derived parameters: LIN (linearity (VSL/VCL)), STR (straightness (VSL/VAP)), WOB (wobble (VAP/VCL)). Explaining these terms here would be beyond the scope of this article.
- The normal valeues are: Velocity more than 46 μ/s and Linearity more than 58 %.
Sperm morphology
Normal values for sperm shape are 4% or more.
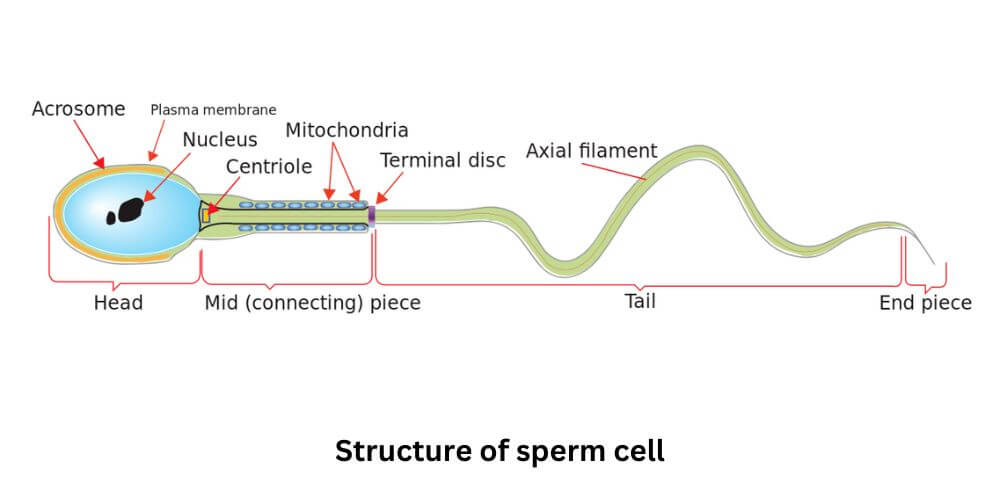
If the percentage of sperms with normal shape is less than 4%, then the term used to describe this condition is called teratozoospermia or teratospermia. The cells with abnormal shapes can further be classified on the basis of defects: head defects, mid-piece defects, and tail defects. Only normal cells contribute to fertility. Attached below is an image of the structure of the sperm cell for your reference.
WBC (White Blood Cells)
The presence of WBCs in semen is called leukocytospermia. Normal values for WBC in seminal plasma are 1 million/ml. The presence of WBC in the seminal plasma is indicative of infection. WBCs can damage the sperm and weaken its genetic material.
RBC (Red Blood Cells)
The condition in which RBCs are present in seminal fluid is called hematospermia. This is indicative of inflammation, injury, and/or blockage anywhere in the male reproductive system.
Biochemical analyses of seminal fluid
Fructose
The normal range is 5 – 30 mM. It is the source of energy for sperm’s viability, function, and motility. Fructose is secreted mainly in seminal vesicles. Low levels of fructose in seminal plasma may indicate the absence of seminal vesicles, dysfunction of seminal vesicles, or obstruction of the ejaculatory ducts.
Alpha Glucosidase
Low levels of alpha-glucosidase accompanied by normal levels of FSH and normal testicular volume may indicate obstruction of the epididymis or vas deferens.
FAQ
What does the sperm analysis tell you
Semen analysis or sperm analysis is one of the tests done to identify and/or confirm the presence or absence of male factor infertility. It is a test done in a laboratory and evaluates sperm count, motility, morphology, and other parameters that are discussed above.
How much sperm is needed for sperm analysis
All of the fluid ejaculated is needed to do the sperm analysis as the volume of semen is one of the evaluating parameters for semen or sperm analysis.
How long does it take for a sperm analysis
Typically, a sperm analysis will take 2-3 business days. Again, this is dependent on where you get your tests done. In Canada it usually takes about 2-4 business days, in the US it takes about 2-3 business days while in India it’s usually about 48 hours or less.
How much does semen analysis cost
It usually costs between 50$ to 200$.
Semen analysis instructions
These instructions are for the patient.
– Patient should observe an abstinence period of a minimum of 48 hours before giving the sample.
– The sample should be given at the laboratory where analysis has to be performed.
– The patient should be mentally prepared since he would be asked to produce the sample by masturbation.
– Patient should be careful to collect all of the ejaculate or not spill or lose any amount of ejaculate.
Semen analysis test at home
There are a couple of test-from-home kits available in the market. The cost of these kits ranges from 50$ – 300$.
Every home test kit available today can not perform all the tests that can be done in a lab. Also, the accuracy of these kits is questionable. I would recommend getting a semen analysis done by a lab.
Image source: Canva (Cover image), public domain (structure of sperm cell)